Use this blog at your own risk
I’m not a doctor, just a writer who has to live with rheumatoid arthritis. I do my best to avoid fake facts, but there’s no guarantee the information in this blog is accurate or up to date. It’s not medical advice or legal advice. So use it at your own risk.
My immune system hates me
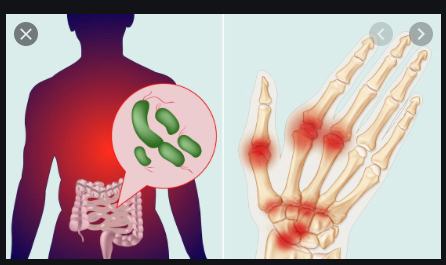
If you have rheumatoid arthritis (RA), (and over 1.3 million Americans do1) you know the drill. When you have a flare, that joint is NOT jumping. For some, inflammation targets the knees and hips or the back and lower legs. For me, it’s usually burning pain and swelling in my hands and wrists. But I can’t stop typing….so what’s a writer to do?
I used to think I had to take my biologic and NSAID, grin, and bear it. But even though doctors still don’t know the exact cause of RA2 new studies show that chronic inflammation is triggered by environmental factors. And surprisingly, diet is one of the most important environmental factors influencing inflammation in RA.3

Figure 1. Arthritic hand of LB. Used with permission.
Ok, think about it
It’s already known that other chronic inflammatory diseases are susceptible to dietary changes. For example, in Crohn’s disease, a plant-based diet may lead to vastly improved symptoms or even remission.4 Similarly, a healthy diet may have the potential to positively influence the symptoms of inflammation in RA.5
You already know what NOT to eat
Research has shown that obesity is an undeniable risk factor for RA. Therefore, avoiding foods that are linked with obesity (i.e., foods high in sugar and unhealthy animal fats known to be linked to inflammation) might be a start to a healthy diet for RA.2
Stop smoking. Lose weight. What else is new?
Losing weight can significantly lower inflammation; the effect can be as significant as someone with RA stopping smoking. Losing weight can help lower the risk of the heart-related complications of RA including high blood pressure, and high cholesterol.2 It’s also linked to a lower degree of joint inflammation.6 Simply losing weight also helps people with RA experience more benefits from their therapy.2
What works, what doesn’t
A study of current literature examined the effect of dietary intervention in RA using a variety of different diets: supervised fasting, the Mediterranean diet, a vegetarian or vegan diet, and the elemental diet (liquids containing nutrients processed to improve digestion).7 The authors concluded that vegan and elimination diets required more studies, while elemental diets did not help patients to improve scores of pain, functional ability, or joint stiffness.8
First, you stop eating. Then you eat, but cut out meat
Several studies have shown that supervised fasting (defined as taking in water but minimal calories for a period of at least 12 hours) minimizes inflammation and pain in RA. Interestingly, inflammation returns when a normal diet resumes, but improvements are maintained when fasting is followed by a vegetarian diet.9,10 So if you want to keep those improvements, it’s time to say sayonara to steak.
Feel the difference FAST when you go veg
People with RA have different guts, literally. The microbes within our GI tracts are peculiar to people with RA and lack the diversity found in the guts of healthy people.6 (See Figure 2 below and for more information and contrasting images, visit http://www.everydayhealth.com)
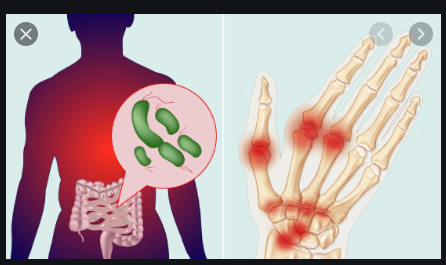
Figure 2. Image copyrighted by Everyday Health http://www.everydayhealth.com
Studies show that changing the microbes in our guts by making healthy dietary changes may lead to better complementary management of RA, if not to remission.6 In these studies, dietary fiber found in plant foods was shown to improve gut bacteria by increasing bacterial diversity, reducing inflammation, and lowering associated joint pain.11
Change begins to be seen and felt within 24 hours….so isn’t that worth a try, at least?
But if you don’t even want to try, consider…
Oldie but goldie..the Mediterranean diet
Some studies have shown that Mediterranean diet food choices are rich in antioxidants. Together with medical therapy, this anti-inflammatory diet may help to alleviate pain and disease activity in RA.12

Figure 3. istock rights free photo
The Mediterranean diet may be particularly appropriate for controlling symptoms of RA because as people grow older and are thus at growing risk for RA, they begin to ‘inflammage’.13 This term has been coined to characterize a state of chronic inflammation that grows as the body ages. It may be caused by increased stressors that lead to high levels of pro-inflammatory mediators.13 Nutritional intervention raises the hope that foods eaten in the Mediterranean diet may help to slow down inflammaging and promote an anti-inflammatory response.14
Star Trek medicine…the wave of the future
Ever hear of a food prescription? You will. Eventually, personalized anti-inflammatory diets using a computerized algorithm to predict response to individual foods and how they are combined into meals may help to manage RA.15
Conclusion
I’m not giving up my biologic and NSAID any time soon. But dietary interventions that reduce inflammation may have a place today in complementary therapy for RA and tomorrow in preventative therapy.16 Intermittent fasting followed by a vegetarian diet or a Mediterranean diet that incorporates olive oil, cooked vegetables, and fish oil may be realistic strategies for people with RA who are ready and willing to incorporate dietary changes into their treatment regimen.16
References:
- https://www.rheumatoidarthritis.org/ra/facts-and-statistics/
- https://www.cdc.gov/arthritis/basics/rheumatoid-arthritis.html
- Skoczynska M, Swierkot J. The role of diet in rheumatoid arthritis. 2018;58(4):259-267.
- Sandefur K, Kahleova H, Desmond AN, et al. Crohn’s disease remission with a plant-based diet: a case report. 2019;11:1385.
- Frisell T, Saevarsdottir S, Askling J. Family history of rheumatoid arthritis: an old concept with new developments. Nat Rev Rheumatol. 2016;12(6):335-343.
- https://www.arthritis.org/health-wellness/treatment/complementary-therapies/supplements-and-vitamins/9-supplements-for-arthritis
- Franeschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci. 2014;69(suppl1):54-59.
- Johansson K, Askling J, Alfredsson L, et al. Mediterranean diet and risk of rheumatoid arthritis: a population-based case-control study. Arthritis Res Ther. 2018;20:175. https://doi.org/10.1186/s13075-018-1680-2
- Hu Y, Costenbader KH, Gao X, et al. Mediterranean diet and incidence of rheumatoid arthritis in women. Arthritis Care Res (Hoboken). 2015;67(5):597-606. doi: 10.102/acr.22481
- Linos A, Kaklamani VG, Kaklamani E, et al. Dietary factors in relation to rheumatoid arthritis: a role for olive oil and cooked vegetables? Am J Clin Nutr. 1999;70:1077-1082.
- Fernandez-Llanio Comella N, Matilla MF, Cuesta JAC. Have complementary therapies demonstrated effectiveness in rheumatoid arthritis? Reumatol Clin. 2016;12(3):151-157. http://dx.doi.org/10/1016/j.reuma.2015.10.011
- Kjeldsen-Kragh J, Haugen M, Borchgrevink CF, et al. Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis. 1991;338:899-902.
- Martucci M, Ostan R, Biondi F, et al. Mediterranean diet and inflammaging within the horesis paradigm. Nutr Rev. 2017;75(6):442-455. doi: 10.1093/nutrit/nux013
- Franeschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci. 2014;69(suppl1):54-59.
- von Schwartzenberg RJ, Turnbaugh PJ. Siri, what should I eat? Cell. 2015;163(5):1051-1052
- Skoldstam L, Hagfors L, Johannsson G. An experimental study of a Meditterranean diet intervention for patients with rheumatoid arthritis. Ann Rheum Dis. 2003;62(3):208-214. https://dx.doi.org/10.1136/ard.62.3.208